INTRODUCTION
The chief advocacy goal of the Medical Society of the State of New York (MSSNY) is to ensure that all New Yorkers can receive quality, accessible and affordable physician-led healthcare. MSSNY advocates for best medical practices for our patients based on science, with a commitment to improving public health and addressing longstanding equity issues in our healthcare delivery system. We represent tens of thousands of physicians and medical students across New York State, including physicians delivering patient care in each of its regions, and those who practice solo, in small groups and large groups, or are employed by a health system.
New York has long held a well-deserved reputation for having a world-renowned health delivery system, but the Covid-19 pandemic challenged us like nothing before. We are hopeful that the worst of the pandemic is behind us, but it has left an indelible mark on many, including our heroic but weary healthcare workforce. Countless physicians on the front lines treating afflicted patients were themselves sickened with the virus. Countless more continue to feel the trauma and other after-effects from the pressures of providing patient care during a harrowing time when hospitals were overwhelmed, and effective treatments were scarce.
Even prior to the pandemic, the excessive administrative hassles in delivering patient care had caused many to suffer from “burnout.” Unfortunately, the pandemic accelerated this disturbing trend. A 2021 Medscape report noted that 51% of critical care physicians reported feeling burnout, as well as 51% of all female physicians, with the overwhelming contributing factor to burnout being too many bureaucratic tasks (58%). Similarly, a 2022 Physician Survey found that 62% of physicians reported feelings of burnout, as compared to 40% pre-pandemic (2018).
Even with the pandemic receding, we are faced with numerous public health threats, some more recent such as MPox and polio, and others that are long-standing. With the demands on our healthcare system growing with an aging population and an increasing number of patients with co-morbid conditions, we must take steps to ensure that we have a physician workforce ready to meet the healthcare demands of our population. This includes reducing the excessive administrative, non-patient care delivery demands that were already driving physician burnout prior to the onset of the pandemic, as well as refraining from enacting well-intended, but often misguided, legislation that adds unnecessary administrative burdens and requirements.
It’s time for a change. New York is regularly ranked near the bottom in the list of the best states in which to practice medicine because of a lack of competitive compensation, excessive regulatory requirements, and excessive liability risk and costs. New York has already lost countless physicians to other states with practice environments more welcoming to physicians.
Replacing physicians with non-physicians is not the answer to this problem. Advanced care practitioners fill essential roles in our healthcare system, but surveys show that most patients want a skilled physician leading the healthcare team. Furthermore, various studies show that physician-led care is more cost-effective. During the 2023 Legislative Session, it is imperative that our policymakers strive to increase and protect New York’s physician workforce, including working to improve New York’s practice environment.
HEALTH INSURANCE REFORM
The Problem
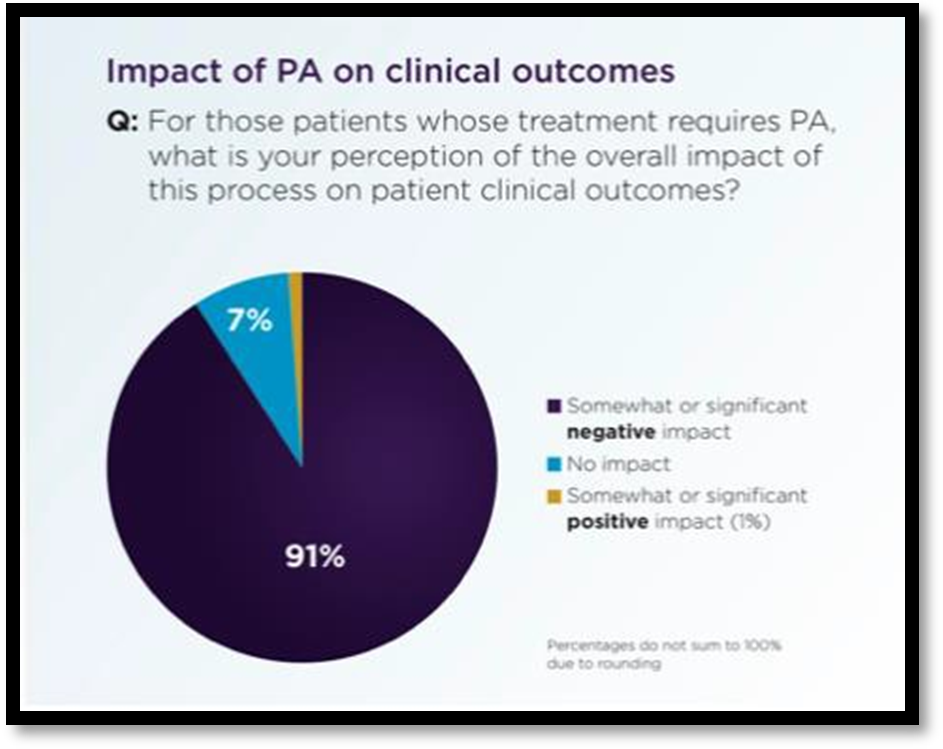
Action is needed to counteract pervasive, health insurer-imposed administrative barriers that interfere with patient care delivery. According to a recent American Medical Association (AMA) survey, 93% of physicians reported care delays because of health-insurer-imposed prior authorization (PA) requirements, while 82% said that PA can lead to patients abandoning their treatments. Moreover, 91% reported that excessive PA burdens have had a negative impact on clinical outcomes, while 88% reported the burden as high, or extremely high.
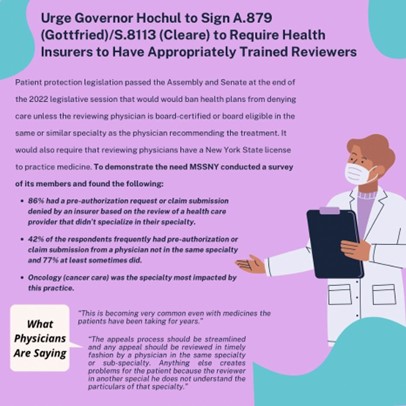
 Adding insult to injury is that health insurers often use insufficiently trained healthcare providers to review PA requests and other claim submissions. A recent MSSNY survey showed that 86% of responding physicians indicated that they had a PA or claim submission denied by a health plan reviewer that was not a physician trained in the same or similar specialty as the physician recommending the care.
Adding insult to injury is that health insurers often use insufficiently trained healthcare providers to review PA requests and other claim submissions. A recent MSSNY survey showed that 86% of responding physicians indicated that they had a PA or claim submission denied by a health plan reviewer that was not a physician trained in the same or similar specialty as the physician recommending the care.
Insurers impose these burdens because of their market dominance. According to the 2021 AMA Competition in Health Insurance: A Comprehensive Study of U.S. Markets, in most regions of New York there are just two insurers that collectively control over 60% of that regional market. Physicians must either accept insurers’ terms or join large health systems to stay in practice and continue to deliver patient care in the communities they serve.
The Solution
To counteract the disproportionate market power of insurers, MSSNY supports the following important reforms:
Prior Authorization (PA) Reform. Recognizing the disproportionate market power of insurers, the legislature directed a workgroup, convened by the New York Department of Financial Services (DFS) and Department of Health (DOH), to reduce administrative burdens in health care. MSSNY actively participated in this workgroup, which recommended a number of modest steps to reduce excessive PA requirements, claims hassles, and delays in credentialing.
Some positive steps were taken by the Legislature in 2022. These include ensuring qualified health plan reviewers of recommended physician care and reducing burdensome step therapy requirements for needed medication. However, even if these bills are signed into law, they only begin to address this overwhelming problem. Far more needs to be done to reduce the hassles that interfere with patient care and exacerbate physician burnout. MSSNY supports the enactment of comprehensive PA reform by the State Legislature. These proposals include:
- Reducing excessive health insurer interference in patient care by exempting physicians and other health care providers from health insurer-imposed PA requirements for a particular health care treatment if previous PA requests to that health insurer for that treatment have been approved at least 90% of the time.
This legislation is similar to a law enacted in Texas last year, known as a “Gold Card” program. It would help to ensure that PA procedures are reserved for those situations that are in need of oversight, permitting the vast majority of physicians to get back to delivering necessary patient care in a timelier manner.
- Streamlining the PA process, and reducing the barriers experienced by patients that inappropriately delay access to needed treatment and medications, by prohibiting repeat PAs where patients are stabilized on such treatment/medication.
Collective Negotiations. MSSNY supports legislation to allow independently practicing physicians to collectively negotiate various contract terms with market-dominant health insurers, including administrative processes such as pre-authorization, step therapy rules, claims payments, and audits of previous payments.
Network Adequacy Reform. MSSNY will advocate for the availability of comprehensive physician networks and protect against unfair narrowing of these networks. To begin with, the Legislature must protect patients against the abrupt loss of access to their treating physicians by ensuring due process protections for physicians when their contracts are not renewed by insurance companies.
Furthermore, to enhance patient access to timely care, reforms should be enacted to improve old standards that DFS and DOH use to determine network adequacy. New standards should be adopted that are comprehensive to meet the health needs of all covered insureds including adding requirements for ensuring appropriate providers in diverse and underserved communities across New York; enhanced transparency, so consumers understand the size and quality of the network to be able to comparison shop; and increased regulatory oversight of incorrect participating physician lists.
 Stronger Enforcement. MSSNY will advocate to ensure aggressive DFS/DOH investigation and enforcement actions against health insurers that engage in patterns of excessive medical record requests that inappropriately delay the payment of routine health care claims. This includes supporting legislation that would enable New York State regulatory agencies to enforce prompt payment laws against self-insured plans. Moreover, with new oversight over the practices of pharmaceutical benefit managers (PBMs), MSSNY will be urging DFS to ensure that formularies and patient cost-sharing requirements are fairly developed and do not create excessive hassles when physicians seek to ensure patients receive necessary medications.
Stronger Enforcement. MSSNY will advocate to ensure aggressive DFS/DOH investigation and enforcement actions against health insurers that engage in patterns of excessive medical record requests that inappropriately delay the payment of routine health care claims. This includes supporting legislation that would enable New York State regulatory agencies to enforce prompt payment laws against self-insured plans. Moreover, with new oversight over the practices of pharmaceutical benefit managers (PBMs), MSSNY will be urging DFS to ensure that formularies and patient cost-sharing requirements are fairly developed and do not create excessive hassles when physicians seek to ensure patients receive necessary medications.
MSSNY will also continue to advocate that New York’s Independent Dispute Resolution (IDR) process maintains its well-deserved reputation of striking a fair balance between the interests of health insurers and healthcare providers in resolving out-of-network surprise medical bills. This includes the continued consideration of Fair Health charge data and maintaining access to IDR to determine fair payment for care provided to patients covered through publicly funded plans.
Supporting Enhanced Insurance Coverage
MSSNY supports efforts to enhance the availability of a mix of affordable and comprehensive health insurance coverage options. This includes limiting the often-astronomical deductibles that exacerbate the problems of patients being underinsured, often hurting diverse and underserved communities. We appreciate the positive steps taken in 2022 to expand eligibility and reduce cost-sharing for various public programs, including raising the income eligibility threshold for New York’s Essential Plan, reducing cost-sharing for CHIP coverage, and expanding Medicaid coverage for mothers and children up to oneyear post-partum. MSSNY supports legislation to further expand access to comprehensive and affordable coverage, including additional tax credits for private health insurance coverage obtained through New York’s Exchange and expanded eligibility for New York’s Essential Plan for all New Yorkers.
Questions Regarding The New York Health Act. While MSSNY has a long-standing position in support of a multi-payer system and in opposition to a single-payer system in New York, we also recognize that the concept is supported by many physicians upset with the excessive administrative hassles of the current multi-payer system. Therefore, we continue to engage with legislators to discuss and evaluate the strengths and weaknesses of any single-payer proposal. Some of the most important questions include:
- Will there still be excessive prior authorization and other administrative hassles associated with providing needed patient care and being timely paid for that care?
- Will there be a fair payment schedule that incentivizes physicians to stay in New York rather than move to other states?
- What would occur if there were substantial state budget shortfalls?
We appreciate that versions of this legislation have sought to provide some answers to these questions. However, there have been numerous instances over the past several years where the medical community has had to strenuously advocate to prevent a patient–access–to–care crisis by fighting the implementation of proposed steep Medicare and Medicaid cuts, in response to federal or state budget shortfalls. It is certainly foreseeable that a similar situation could occur under a singlepayer system. It is imperative that these concerns be addressed as part of any single-payer proposal.
CONTAIN EXORBITANT MEDICAL LIABILITY COSTS
 Physician practices are still recovering from the financial strain of the pandemic. This strain heightens the need to contain New York’s notoriously excessive liability costs.
Physician practices are still recovering from the financial strain of the pandemic. This strain heightens the need to contain New York’s notoriously excessive liability costs.
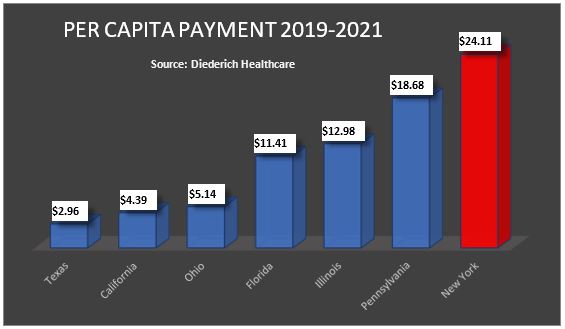
Unfortunately, New York’s physicians and hospitals continue to incur the highest liability awards and costs in the nation, far surpassing more populous states such as California and Texas. Medical liability costs hurt consumer affordability and access, as these costs contribute to New York’s high premium costs, which also limit small business growth. Moreover, excessive liability costs disproportionately impact physicians working in underserved communities who have experienced heightened financial strain from the pandemic. For these reasons, New York is regularly ranked worst among states in the country for physicians to practice medicine.
If that were not bad enough, this past year the New York State Legislature passed a bill (A.6770/S.74-A) that could significantly increase New York 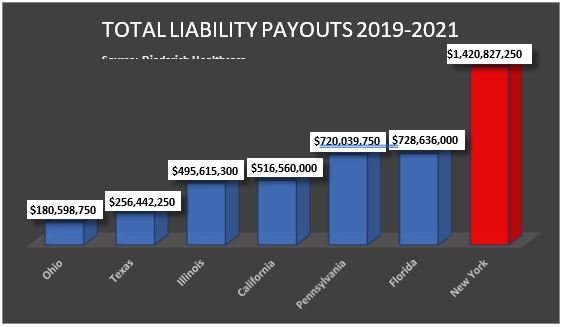 physicians’ already astronomical medical liability premiums by expanding the types of damages awardable in a wrongful death action. One actuarial study concluded that it would require premium increases of nearly 40%.
physicians’ already astronomical medical liability premiums by expanding the types of damages awardable in a wrongful death action. One actuarial study concluded that it would require premium increases of nearly 40%.
MSSNY has argued that legislation to expand liability should only be considered in the context of a comprehensive effort to address New York’s excessive liability costs. While many other states have passed laws to contain medical liability payouts and provide greater fairness in medical liability litigation, New York has not, which is why our medical liability insurance and payout costs far exceed every other state in the country.
MSSNY Supports legislative initiatives to reduce malpractice costs and non-meritorious claims, including many that have proven successful in dozens of other states, such as:
- Certificates of Merit. Expanding New York’s existing flimsy Certificate of Merit requirement to require that a more detailed justification be provided for filing a medical malpractice lawsuit. This is particularly important given that roughly 2/3 of all medical liability actions result in no payment to the plaintiff, yet tens of millions of dollars are spent on defense costs, each year, for these non-meritorious claims.
- Expert Witnesses. Requiring that an expert witness in a medical malpractice action practice in the same specialty as the defendant physician.
- Ensuring statements of apology from a physician to a patient are not ‘discoverable’ in future litigation.
- Reasonable Damages. Placing reasonable limits on non-economic damages, as have over 30 other states across the country including California and Texas.
- Alternative Resolution. Creating alternative systems for resolving liability claims such as medical courts or a Neurologically Impaired Infants Fund.
- Protecting Excess Malpractice Coverage. Continuing an adequately funded Excess Medical Malpractice Insurance Program without imposing cost-sharing requirements on physicians receiving this essential coverage.
MSSNY Opposes various stand-alone measures that could further increase malpractice insurance costs, such as:
- Anti-Consumer Attorney Fee Increases. Oppose the elimination of statutory consumer protections against exorbitant attorney contingency fees.
- Pre-Judgment Interest. Permitting the awarding of interest from the date of the lawsuit, rather than the court decision or date of settlement. NY’s judgment interest rate is 9%, far above usual interest rates.
- Pre-Trial Cost-Sharing. Oppose proposals to force litigants in multi-defendant actions to make decisions before trial regarding post-verdict cost-sharing.
- Reducing Defense Rights. Oppose the elimination of important defense rights that would limit the ability of a defendant physician’s counsel to question plaintiff’s treating provider.
Protecting Care Improvement Efforts through Peer Review. MSSNY continues to support efforts to enhance healthcare quality improvement by encouraging open dialogue in hospital peer review proceedings without fear that such statements may be used against them in litigation. An absurd exception to New York’s peer review confidentiality law permits the discovery by trial lawyers of statements made by a physician during peer review who subsequently is sued. This naturally discourages the full and frank discussion of efforts to improve care delivery. This long-standing problem was further exacerbated by a recent 2nd Department judicial decision (Siegel v. Snyder) that further limited the confidentiality of all peer review discussions where the identity of the speaker cannot be discerned. Because New York’s excessive liability environment discourages open communication of healthcare delivery, confidentiality of efforts to learn from adverse events in care delivery is essential. To address this problem, MSSNY supports legislation to ensure that peer review discussions can be robust without fear of litigation by ensuring its confidentiality.
PRESERVING AND ENHANCING PHYSICIAN-LED TEAM-BASED CARE
To ensure patients receive the highest quality care, MSSNY supports efforts to preserve the physician-led care model in healthcare settings across the state. Our patients are best served by the combined care of a team, led by a physician whose education and training enables them to oversee the care to ensure optimal medical treatment for the patient. Maintaining and promoting physician-led healthcare is not only critical for the health and well-being of patients, but also what they want. A recent national survey reported that 95% of patients believe it is important that a physician be involved with their diagnosis and treatment decisions.
Training. Ensuring treating professionals are acting within their scope of practice is also a matter of patient safety. Most physicians must complete 4 years of medical school plus 3-7 years of residency and fellowships, including 10,000-16,000 hours of clinical training before they are permitted to treat patients independently. During this training physicians receive approximately 5,000 hours of clinical experience in medical school, 4,000 hours of clinical experience in internship, and 6,000 to 18,000 clinical hours during specialty training. This extensive training makes physicians best suited to deliver and coordinate needed primary and specialized patient care.
As New York is regularly identified as one of the worst states in the country to practice medicine due to excessive liability costs and lack of competitive payment, there are shortages of physicians in many parts of our state. Unfortunately, some have used this shortage as a justification to expand the scope of healthcare services that can be provided by various non-physicians without required collaboration with a trained physician. The solution to this physician shortage is to make New York a more welcoming environment for physicians to deliver patient care, not expanding the scope of practice for non-physician providers.
Concerns. MSSNY has repeatedly expressed grave concerns with various Governor’s Executive Orders (EO) that waived otherwise applicable statutory collaboration and supervision requirements for nurse practitioners (NPs), physician assistants (PAs), and nurse anesthetists (CRNAs). A recent MSSNY survey reported that 75% of the physician respondents indicated that the advanced care practitioners working independently since the issuance of these EOs had committed an error while treating a patient. Furthermore, 90% of physicians indicated that the error could have been prevented had there been physician oversight.
The Cost-Effectiveness of Physician-Led Team Care. A recent AMA study finds that when non-physicians are permitted to practice independently, this difference in training results in increased healthcare costs and patient safety risks. An examination of 10 years of cost data on 33,000 patients by the South Mississippi system’s Accountable Care Organization of physicians and independently practicing PAs and NPs found that NPs and PAs ordered more tests and referred more patients to specialists and hospital emergency departments than physicians. Moreover, the data also showed that physicians performed better on nearly all quality measures, including double-digit differences in flu and pneumococcal vaccination rate.
Furthermore, proposals to sever existing collaborative and supervisory requirements could result in increased healthcare costs due to overprescribing and overuse of diagnostic imaging. One study in the Journal of the American College of Radiology analyzing skeletal x-ray utilization for Medicare beneficiaries over 12 years found ordering increased substantially – more than 400% by non-physicians, primarily NPs and PAs during this period. Another study published in JAMA Internal Medicine found NPs ordered more diagnostic imaging than primary care physicians following an outpatient visit.
Legislation. Given these concerns, MSSNY Opposes legislation that would create healthcare silos, including by:
- Inappropriately permitting independent practice for CRNAs.
- Inappropriately permitting independent PA practice including to perform fluoroscopy.
- Inappropriately expanding the authority of NPs to deliver care without collaboration by physicians practicing in the same specialty as the NP.
- Inappropriately expanding the ability of podiatrists to treat up to a patient’s knee.
- Inappropriately permitting pharmacists to order and conduct patient lab tests without physician coordination.
- Inappropriately granting psychologists prescribing privileges.
At the same time, MSSNY supports the ability of otolaryngologists to dispense hearing aids at fair market value. With the federal government authorizing the sale of hearing aids over the counter, there is no logical reason to maintain an artificial distinction between which providers can sell hearing aids for profit. Moreover, MSSNY supports “Truth in Advertising” legislation that would ensure that all healthcare providers be required to conspicuously identify their type of state license when treating patients in all healthcare settings, as well as in advertisements to the public.
ADDRESSING OUR PUBLIC HEALTH NEEDS
Infectious Disease Outbreaks and Prevention
For the first time in its history, our state is dealing simultaneously with three infectious disease outbreaks: COVID-19, MPox, and polio. Throughout the height of the Covid-19 pandemic, as well as the MPox and polio outbreaks, MSSNY’s Committee on Emergency Preparedness and Disaster/Terrorism Response has educated physicians on how they can work best with the State’s public health infrastructure to prevent the spread of these communicable diseases, including through regular meetings with the NYS Department of Health (DOH) and other local public health agencies.
COVID-19. The COVID-19 pandemic has reshaped so many aspects of our lives —from health habits and work environments to social norms. The World Health Organization still classifies the COVID-19 pandemic as an acute global emergency. Many governments face uncertainties about how to prioritize at a time when the pandemic appears to be in transition but when the risk of emergence of new variants and future surges remains real. In the United States, many people have some protection, or immunity, against COVID-19 due to vaccination, previous infection, or both. This immunity, combined with the availability of tests and treatments, has greatly reduced the risk of severe illness, hospitalization, and death from COVID-19 for many people. At the same time, some people—such as those who are older, are immunocompromised, have certain disabilities, have certain underlying health conditions, or who live in underserved communities—continue to be at higher risk for serious illness.
COVID-19 immunizations have played a significant role in mitigating the loss of life from the virus. New York’s immunization rate is 79% for adults and children. The new boosters that include the BA variants will provide continued protection. MSSNY supports mandatory COVID-19 vaccination among all school-aged children, now that the Centers for Disease Control and Prevention (CDC) and U.S. Food and Drug Administration (FDA) have confirmed the safety and efficacy of the COVID-19 vaccines in the pediatric population. MSSNY also supports a requirement for the administration of the influenza vaccine for all school-age children who attend childcare, pre-kindergarten, K-12, and college and universities in New York State, unless medically contraindicated. The American Academy of Pediatrics (AAP) also supports this requirement.
MPox. MPox is a rare, viral infection that can result in hospitalization or death. MPox spreads through close, physical contact between people. Based on the current outbreak, certain populations are affected by MPox more than others, including men who have sex with men. Based on previous outbreaks of MPox around the world, some groups may also be at heightened risk for severe outcomes if they contract MPox. This includes people with weakened immune systems, the elderly, children under 8 years of age, and the pregnant. In New York State there are approximately 4,000 cases of MPox. There is a vaccine licensed by the FDA as a two-dose series for the prevention of MPox among adults ages 18 years and older. Statewide eligibility currently includes the following New Yorkers: individuals with recent exposure to a suspected or confirmed MPox case within the past 14 days; those at high risk of a recent exposure to MPox, including gay men, members of the bisexual, transgender, and gender non-conforming community, and other communities of men who have sex with men; individuals who have engaged in intimate or skin-to-skin contact with others in the past 14 days in areas where MPox is spreading; individuals who have had skin-to-skin contact with someone in a social network experiencing MPox activity, including men who have sex with men who meet partners through an online website; and any individual that may be at risk of future exposure to infection withMPox.
Polio. Successful vaccination campaigns in the 1950s resulted in poliovirus being declared eliminated in the United States in
- However, the case of an individual paralyzed by polio and the finding of the virus in wastewater in the lower Hudson Valley and New York City has resulted in a new immunization program for 2-year-old children by the NYS DOH, in collaboration with the local health departments.
Promoting Immunizations
Prevention of diseases continues to remain a top MSSNY priority and the best way to prevent or ameliorate the severity of these diseases, including COVID-19, MPox, and polio is through immunizations. Vaccines are safe and effective—and they save lives. Vaccination programs have allowed us to “get back” some normalcy during the pandemic and they have helped organized medicine and the state combat MPox and polio outbreaks.
The vaccination of school-age children, teens, and young adults promotes herd immunity. This protects elderly populations and the immunocompromised who are at highest risk of serious complications of influenza. Therefore, MSSNY supports an influenza and COVID-19 vaccine requirement for all school-age children who attend childcare, pre-kindergarten, K-12, and college and universities in New York State, unless medically contraindicated.
In 2019, MSSNY together with many other groups supported a law to require that every child attending a public, private or parochial school receives the appropriate immunizations, except where there is a medical contraindication. However, our State has seen an increase in the number of medical exemptions issued to school-age children from vaccination requirements. MSSNY has strongly encouraged physicians to follow the CDC guidance when issuing a medical exemption and has reminded that falsely certifying a medical exemption form could result in a disciplinary action.
Needed Public Efforts. Vaccination doesn’t just protect those receiving the vaccine. Critically, vaccines help to prevent spread to others, including infants who are too young to be vaccinated and those who are unable to receive a vaccine due to a health condition. MSSNY continues to support state funding for a public health campaign to promote immunizations to educate “vaccine-hesitant” individuals. MSSNY also supports requiring all public, private, and parochial schools in New York State and New York City to report immunization rates and medical exemptions to one central NYS Department of Health database, to help effectively track immunization rates throughout the state.
MSSNY supports universal reporting of adult immunizations to the New York State Immunization Information System (NYSIIS), either directly or via health information exchanges, and supports removing the requirement for patient permission to report adult vaccines to the registry.
Improving Women’s Health
In light of the decision by the U.S. Supreme Court to overturn Roe v. Wade, preserving the right for women to have access to reproductive and sexual health care services is even more critical. Abortion has been legal under New York State law since 1970 – three years before the Roe v. Wade decision. MSSNY is strongly opposed to any federal or state legislation that would prohibit physicians from exercising clinical judgment in the delivery of medical care, and strongly supported legislation enacted this year to protect physicians from legal sanctions in New York for providing needed patient care illegal in other states, but legal in New York. MSSNY supports legislation and other efforts to expand access to emergency contraception, including making emergency contraception more readily available, and will continue to support sexual health education programs amongst adolescents.
Reducing Substance Abuse
MSSNY actively works to increase physician awareness and leadership to combat the opioid and pain crisis and supports efforts to expand access to MAT (medications for addiction treatment) including methadone for patients with opioid use disorders.
As we continue to confront the problem, it is important to note the enormous progress that has been made. According to data provided by IQVIA, prescription opioid volume dropped 46% in the US between 2012 and 2021, and in New York decreased by nearly 50%. Certainly, this progress is the result of comprehensive efforts by many, including the physician community, to better ensure that the prescribing of pain medications is appropriate to the patient’s needs. Concurrently, the New York Legislature enacted numerous measures to further regulate opioid prescribing, including a 2012 law to require consultation with the I-STOP database prior to a controlled substance prescription; and a 2016 law to require all DEA-registered prescribers to take Continuing Medical Education coursework on pain management and limiting initial acute pain medication prescriptions to 7 days. MSSNY is currently revising this course to keep it up to date with changes in the law on the state and federal levels and to address the revision of the CDC chronic pain guidelines.
Protecting Against Unintended Effects. It is also important to ensure that efforts to address one problem do not create another. We must protect against the misapplication of rigid guidelines. In 2018, a law was enacted in New York to require all prescriptions for treating patients’ chronic pain to be consistent with CDC chronic pain guidelines. These CDC guidelines are themselves being revised to address the unintended effect that physicians were reluctant to appropriately prescribe opioids to relieve patients’ pain because of a fear of prosecution by disciplinary bodies. As a member of the AMA Substance Use and Pain Care Task Force, MSSNY strongly supports the changes to the CDC guidelines including the removal of specific dosage and day limits for an opioid prescription and the emphasis on patient-physician shared decision-making, largely absent from the 2016 guidelines. MSSNY and the AMA expressed their appreciation to the CDC for acknowledging that the rigid limits of the 2016 guidelines were widely misapplied and resulted in widespread harm to patients with pain, including care delayed and denied, and even death by suicide. We also appreciate that the CDC has acknowledged the harm caused by an inappropriate focus on “pain as the fifth vital sign.”
Confronting the Realities of Recreational Marijuana. With the implementation of legalized cannabis, MSSNY continues to support efforts to protect the public from inappropriate marketing tactics that could lead to substance abuse. According to a SAMHSA 2019 National Survey of Drug Use among people aged 12 or older, the percentage who were marijuana users in the past year increased from 11% (or 25.8 million people) in 2002 to 17.5% (or 48.2 million people) in 2019. The report also said that among people aged 12 or older, the number of past year initiates of marijuana use increased from 2.2 million people in 2002 to 3.5 million people in 2019. Among those 12-17, perceived great risk of harm from smoking marijuana weekly declined from 40.6% in 2015 to 34.6% in 2019.
Safe Injection Facilities. MSSNY supports the creation of pilot studies to assess the role of Safe Injection Facilities and that pilot locations include New York City and two other areas outside NYC. Additionally, MSSNY advocates that these pilot studies provide screening, support, and referral for treatment of substance use disorders and co-occurring medical and psychiatric conditions, and provide education on harm reduction strategies including Naloxone training.
End-of-Life Care
Challenging decision-making concerning end-of-life care has increased the burden on physicians, patients, and family members. These challenges have divided family members, physicians, and the social fabric of society. When intimate knowledge of end-of-life choices have not been discussed between doctor and patient, an ever-changing medical environment with shifting social mores, economic influences, and legislative mandates can muddle already difficult medical decisions. Further complexities arising from an acute crisis in the use of narcotic analgesics have also frustrated patients and providers in dealing with prevention and relief of pain at end of life. To address these challenges, MSSNY supports:
- Developing a state central depository for eMOLST (Medical Orders for Life Sustaining Treatment) forms.
- Requiring adequate reimbursement for end-of-life care.
- Expanded options for obtaining affordable long-term-care insurance.
- Urging NYS DOH to develop educational resources for physicians, allied professionals, and patients on end-of-life care.
- Urging NYS DOH to simplify the hospice recertification process.
Reaffirming MSSNY Policy 95.989 in opposition to Physician Assisted Suicide and Euthanasia.
ADDRESSING PHYSICIAN WELLNESS AND SYSTEMIC STRESSORS
For years, physicians have become increasingly demoralized by the systemic stressors that have fueled the burnout crisis in healthcare. Factors including increasing regulatory requirements, administrative and record-keeping burdens, chasing and documenting unproven measures, and liability issues have resulted in growing work hours and time in front of a computer screen instead of interacting with patients. These factors have caused rising levels of dissatisfaction for both patients and physicians. Physician burnout has also been linked to lower productivity, absenteeism, medical errors, and less effective healthcare teams.
The outbreak of COVID-19 further tested the resiliency of New York’s physicians, residents, and medical students as never before. A 2022 report by The Physicians Foundation indicated that more than two years into the pandemic, the state of physician well-being has worsened and burnout rates have increased from 40% to 60%. The report found that most physicians have struggled with anxiety, tearfulness, or anger, and half of physicians believe that demoralization and burnout are affecting their peers and themselves at work. Over 1/3 of doctors report that they have had to check on a colleague they believed was in distress. Moral injury, a concept first discussed in the military, involves a deep emotional/spiritual wound unique to those who witness intense human suffering, choices and actions that are harmful, or loss of control when bad things happen. Through peer-to-peer and wellness interactions, we are seeing NY physicians struggle with demoralization and moral injury. On a positive note, about 57% of physicians found peer-to-peer support groups to be helpful.
Promote Peer Support (MSSNY P2P). Physician suicide is a growing professional and public health concern. Despite working to improve the health of others, physicians often sacrifice their own well-being to do so. Furthermore, there are systemic barriers in place that discourage self-care and help-seeking behaviors among physicians. The suicide rate among the profession has exploded in recent decades. The suicide rate among male and female physicians is 1.41 and 2.27 times higher than that of the general male and female populations, respectively.
In response, MSSNY has implemented a Peer-to-Peer (P2P) program that offers an opportunity to talk with a peer about some of life’s stressors. The MSSNY P2P program allows trained peer supports to assist their colleagues who need help in dealing with work, family stressors, and COVID-19. To further enable this program, MSSNY supports legislation to facilitate the ability of physicians to have therapeutic “peer-to-peer” conversations by providing confidentiality protection for organizations and individuals that provide physician peer support, like protections provided to the NYS Bar Association peer support activities.
Continuing the Committee for Physicians Health. MSSNY strongly supports the extension of the Committee for Physicians Health (CPH) program. The program has been in existence for over 40 years, with the current legislative authorization scheduled to expire in June 2023. The CPH is an essential public health program designed to confront and assist physicians thought to be suffering from alcoholism, substance abuse, or mental illness. Since the inception of this program in the 1980s, CPH has assisted thousands of physicians in returning healthy to medical practice and routinely monitors the recovery of 450 physicians.
Steps To Promote Health Equity
In 2021, MSSNY adopted a statement developed by the MSSNY Committee on Health Equity that says in part that MSSNY affirms that racism is a public health crisis and that MSSNY’s mission statement will be evaluated to ensure that it supports equity in all aspects of its work. Furthermore, MSSNY will systematically evaluate its policies and procedures to be clear that it supports equity in all aspects of its work, in both existing and future policies and procedures, and that records of this process will be visible to all members. MSSNY, through its Committee on Health Equity, will seek to:
- Increase awareness of how discrimination based on factors such as racism, classism, cisgenderism, heterosexism, ableism, patriarchy, and xenophobia contribute to both societal and health inequities and to ensure that all New Yorkers receive the best care possible and can achieve the best health possible.
- Work with stakeholders, including the AMA, specialty societies, Albany leadership, community groups, and others to eliminate inequities, particularly those inequities that adversely impact the health, well-being, and access to/quality of care for persons who are from historically disadvantaged populations.
- Prevent and manage diseases that are prevalent in historically disinvested populations burdened with the worse disease outcomes, including diabetes, hypertension, and cancer, through educational programming for physicians and other stakeholders. MSSNY will also advocate for fair payment for treatment of such conditions.
- Reverse the troubling increases in race/ethnic-based health inequities such as maternal mortality; and promote expanded funding for programs that attract a more diversified physician workforce, increasing the number of minority faculty including female, Black, Latinx, Native American, LGBTQ, and faculty with disabilities teaching in medical schools. MSSNY will also work to expand medical school pipeline programs in rural and urban areas to address the shortage of physicians in medically underserved areas of New York.
Support gender-affirming care by advancing the ability of physicians in New York to provide gender-affirming care to people including transgender and non-binary youth and opposing the criminalization of gender-affirming care for youth.
STEPS TO PROMOTE HEALTH EQUALITY
In 2021, MSSNY adopted a statement developed by the MSSNY Committee on Health Equity that says in part that MSSNY affirms that racism is a public health crisis and that MSSNY’s mission statement will be evaluated to ensure that it supports equity in all aspects of its work. Furthermore, MSSNY will systematically evaluate its policies and procedures to be clear that it supports equity in all aspects of its work, in both existing and future policies and procedures, and that records of this process will be visible to all members. MSSNY, through its Committee on Health Equity, will seek to:
- Increase awareness of how discrimination based on factors such as racism, classism, cisgenderism, heterosexism, ableism, patriarchy, and xenophobia contribute to both societal and health inequities and to ensure that all New Yorkers receive the best care possible and can achieve the best health possible.
- Work with stakeholders, including the AMA, specialty societies, Albany leadership, community groups, and others to eliminate inequities, particularly those inequities that adversely impact the health and well-being and access to and quality of care for persons who are from historically disadvantaged populations.
- Prevent and manage diseases that are prevalent in historically disinvested populations burdened with the worse disease outcomes, including diabetes, hypertension, and cancer, through educational programming for physicians and other stakeholders. MSSNY will also advocate for fair payment for treatment of such conditions.
- Reverse the troubling increases in race/ethnic-based health inequities such as maternal mortality; and promote expanded funding for programs that attract a more diversified physician workforce, increasing the number of minority faculty including female, Black, Latinx, Native American, LGBTQ, and faculty with disabilities teaching in medical MSSNY will also work to expand medical school pipeline programs in rural and urban areas to address the shortage of physicians in medically underserved areas of New York.
- Support gender-affirming care by advancing the ability of physicians in New York to provide gender-affirming care to people including transgender and non-binary youth and opposing the criminalization of gender-affirming care for